The Allergy & Clinical Immunology Fellowship Training Program is designed to provide sophisticated advanced training in the discipline following the completion of an Internal Medicine and/or Pediatric Residency.
Graduates of the program will be proficient in the delivery of care to patients with allergic and immunologic diseases and be prepared to conduct independent research in the field. The program is two years in length and includes clinical and research components. Clinical experience comprises 50% of the total time, with a minimum of 25% research. With close faculty mentorship, trainees choose, design and complete either a focused clinical or bench research project and present their research findings at national meetings and in peer-reviewed publications. In addition, a minimum of three weekly didactic lectures and/or literature review sessions provide further educational experience.
Fellows are provided with direct patient care of new and established patients in the inpatient and outpatient settings, with cross training in Internal Medicine and Pediatric Allergy and Immunology. Outpatient clinical training is conducted at multiple University of Michigan Allergy Clinics, the Corner Health Center, and the VA Ann Arbor Healthcare System. Inpatient clinical training is conducted at the University of Michigan Hospital and spans 12 of the 24 months of the fellowship. Fellows are trained on a variety of core allergy procedures, as well as specialized training in nasopharyngoscopy. Required clinical electives include:
- Otolaryngology
- Adult Pulmonary - COPD Clinic
- Pediatric Dermatology
- Allergen Extract Lab
- Clinical Diagnostic Immunology Lab
Fellows are provided with a structured research experience resulting in an understanding of basic principles of study design, performance, analysis, and reporting. This activity will comprise 6-12 months of the 2-year fellowship. During this time, fellows will:
- Identify a research mentor, conduct a comprehensive literature search and design, write, review, and edit a research protocol or plan
- Attain a working understanding of research design, statistics, clinical trials, epidemiology, and laboratory research
- Acquire a working knowledge of research-based ethics and principles of confidentiality
- Be able to apply the principles of data collection, data analysis, and data interpretation
- Conduct the research activity under proper supervision
- Communicate research findings orally and in writing semi-annually
- Upon completion of their research, submit a manuscript to the Program Director for review
In addition to clinical and research training, fellows will engage in several other scholarly activities. These activities are designed to encourage innovative educational experiences within the program and include, but are not limited to, the following:
- Preparation of and attendance at didactic sessions – case conferences, seminar presentations, dinner rounds, and journal clubs
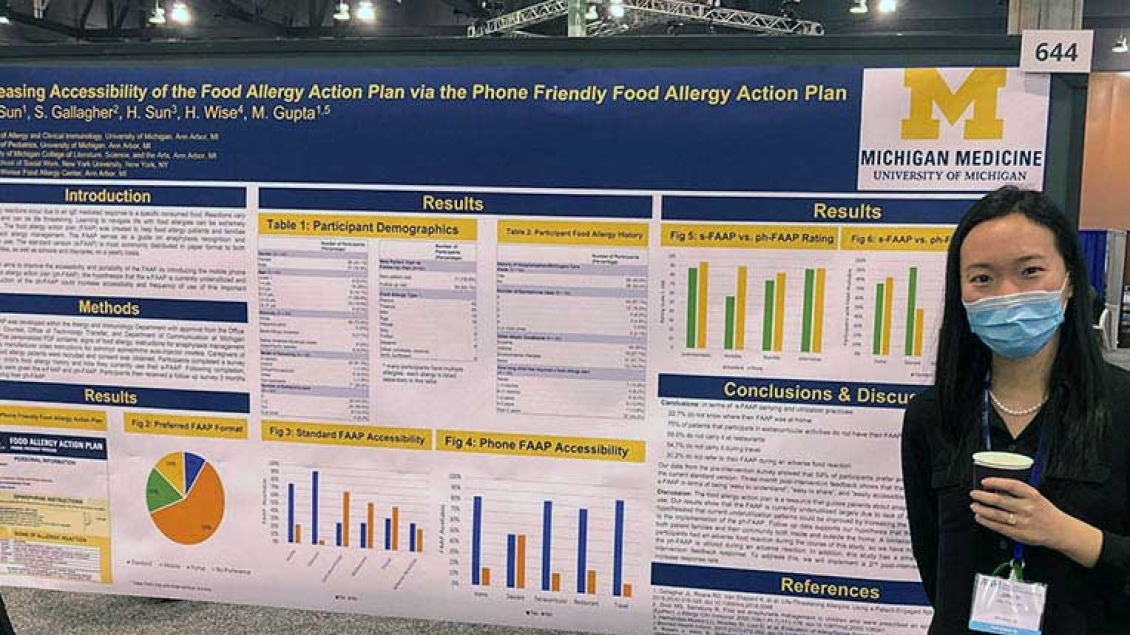
- Presentations and attendance at required national meetings
- Committee work and time devoted to administrative requirements of the hospital
- Committee work within the hospital and/or with other health organizations
- Scientific writing
Fellows are required to communicate their knowledge to others, both orally and in written form, to conduct seminars and clinical conferences, and to prepare written reports of their research activities for faculty review and publication.
Upon completion of the Allergy and Clinical Immunology Fellowship Training Program, fellows will be prepared to sit for the ABAI certifying exam.
In conjunction with the above activities, residents will obtain Allergy/Immunology specific competence in the six areas listed below to the level expected of a new practitioner:
- Patient care that is compassionate, appropriate and effective for the treatment of health problems and the promotion of health
- Medical Knowledge about established and evolving biomedical, clinical and cognate sciences, as well as the application of this knowledge to patient care
- Practice-based learning and improvement that involves the investigation and evaluation of care for their patients, the appraisal and assimilation of scientific evidence, and improvements in patient care
- Interpersonal and communication skills that result in the effective exchange of information and collaboration with patients, their families and other health professionals
- Professionalism, as manifested through a commitment to carrying out professional responsibilities, adherence to ethical principles and sensitivity to patients of diverse backgrounds
- Systems-based practice, as manifested by actions that demonstrate an awareness of and responsiveness to the larger context and system of health care, as well as the ability to call effectively on other resources in the system to provide optimal health care