-
Education Hub -
Medical Student Programs -
Residency -
Fellowships & Advanced Training Programs -
Cancer Genetics & Breast Health -
Complex Family Planning -
Global Women's Health -
Gynecologic Oncology -
Hospitalist -
Maternal Fetal Medicine -
Minimally Invasive Gynecologic Surgery -
Pediatric & Adolescent Gynecology -
Reproductive Endocrinology & Infertility -
Urogynecology & Pelvic Reconstructive Surgery -
Women's Health
-
-
Opportunities -
Facilities & Spaces

The goal of the Advanced Training Program in Minimally Invasive Gynecologic Surgery (MIGS) is to provide trainees with the necessary knowledge, skills, and experience to become outstanding clinicians, teachers, and research contributors.
Learn more by jumping to the sections below:
The University of Michigan Advanced Training Program in Minimally Invasive Gynecologic Surgery (MIGS) is a two-year program that prepares gynecologic surgeons to be experts in complex gynecology, advanced laparoscopic, and minimally invasive surgical techniques. Our program has been accredited by the American Association of Gynecologic Laparoscopists (AAGL) since 2005.
Our faculty and trainees perform the highest number of laparoscopic and robotic hysterectomies and myomectomies and have the greatest experience in minimally invasive surgeries for benign conditions in the region.
Trainees actively participate in all aspects of inpatient and outpatient care of patients seen by our MIGS faculty and receive one-on-one training in the evaluation and management of complex gynecology patients.
MIGS Specialty Clinics:
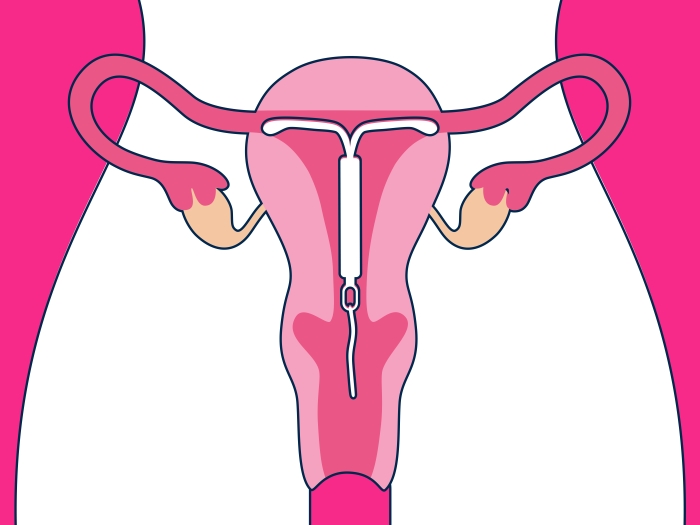
Trainees spend approximately 1 – 1.5 days in specialty MIGS clinics, including the Minimally Invasive Surgery Referral Clinic, the Endometriosis Center, and the Pelvic Pain Consultative Clinic. Through this experience, trainees acquire valuable exposure to the minimally invasive approach to common gynecologic complaints such as abnormal uterine bleeding, uterine fibroids, and adnexal masses. Trainees will also gain extensive experience in the multi-system and multidisciplinary approach to the evaluation of chronic pelvic pain and endometriosis.
Surgical Experience:
Trainees spend approximately 2-3 days in the operating room, taking a hands-on role in all surgical cases performed by the MIGS faculty. In addition to time spent in the operating room, trainees will further refine their skills in surgical simulation labs and cadaver labs done jointly with GYN oncology and urogynecology.
Off-Service Rotations and Electives:
All MIGS trainees at U-M Medical School will have the opportunity to spend one month each year on the gynecologic oncology service. During these rotations, our trainees participate in both the medical and surgical care of patients and gain important exposure to the preoperative evaluation, screening, and evaluation of gynecologic malignancies. Additional elective time can be used to rotate in outpatient clinics within urogynecology, vulvar disease, and advanced pain care.
U-M Medical School is recognized as one of the premier residency programs in obstetrics and gynecology in the United States, and MIGS trainees play an integral role in the education of residents and medical students within the department. One resident (PGY3 or PGY4) and one or more medical students are assigned to the division for each rotation. In addition to teaching on daily work rounds and in the operating room, trainees are asked to prepare and deliver formal lectures and seminars for the resident core curriculum and to lead the discussion at department journal clubs.
Trainees have numerous opportunities to receive formal training and mentorship in research, including a structured statistical curriculum for all ACGME and non-ACGME trainees. An important ancillary goal of the two years of clinical training is to provide a framework in which the trainee can learn to balance the demands of clinical care with those of scholarly pursuits, including ongoing clinical research and manuscript preparation.
Under the supervision of the Program Director, trainees will be expected to complete one independent research project, culminating in a presentation at a national meeting and at least one publication in a peer-reviewed journal. Research time will be allocated on a weekly basis according to the service month, and semi-weekly MIGS division research meetings will serve as the forum to discuss and review the progress of trainee projects.
Sample Research Timeline:
A sample research timeline for appropriate progression for our two-year program is as follows:
- Phase 1: Year 1 (August – September)
- Identify Research Question
- Review the literature and establish a relevant and important research question
- State testable hypothesis and specific aims of the study
- Identify Research Question
- Phase 2: Year 1 (October – November)
- Design research study and methods
- Submit IRB
- Phase 3: Year 1-2 (January – December)
- Collect data
- Phase 4: Year 2 (January – June)
- Analyze results
- Prepare manuscripts for publication
Over the course of the program, all trainees will participate in weekly MIGS didactic sessions. Reading material on a clinical topic is assigned to the trainees and is supervised by the MIGS faculty. Particular attention will be given to areas of controversy and new research and include the AAGL core reading articles. Topics to be discussed will closely follow the AAGL FMIGS educational objectives and will utilize the most recent literature and/or textbooks, including but not limited to the AAGL FMIGS reading list.
Trainees will also participate in a monthly Interdisciplinary Deep Endometriosis Conference with the MRI radiology team to review clinical cases and published literature and develop research studies and protocols for deeply infiltrative endometriosis.
In addition, our Department hosts weekly Grand Rounds and Morbidity and Mortality conferences.
The Department is home to 11 Board-certified and non-Board-certified clinical and research fellowships in obstetrics and gynecology. To promote cross-specialty collaboration, all trainees take part in our didactic curriculum. These are ½ day educational seminars on numerous topics relevant to clinical research and academic leadership.
Topics include research design and implementation, identifying funding opportunities, manuscript timelines and preparation, how to be an effective teacher and employment opportunities. In addition, the department sponsors social events for fellows and advanced trainees across all specialties to further encourage collaboration and to help fellows build both a professional and personal network.
The U-M Medical School Department of Obstetrics and Gynecology is committed to the ongoing development and education of our faculty, staff, and learners. Each year, we provide over 100 CME activities for physicians and healthcare professionals to enhance learning and improve patient outcomes.
Minimum Requirements
- Completion of a residency program accredited by ACGME, College of Family Physicians of Canada, Royal College of Physicians and Surgeons of Canada, or National Joint Committee on Accreditation of Pre-registration Physician Training Programs of the Canadian Medical Association
- USMLE/COMLEX scores
Due to Department of Labor prevailing wage regulations, we are unable to consider applicants that possess any type of visa.
Application Deadline
The application deadline for an August 2025 start date is Wednesday, May 1, 2024. Invitations will be extended on Friday, May 24, 2024. Virtual interview dates will be Tuesday, August 27, 2024, and Tuesday, September 3, 2024.
How to Apply
Applications are only accepted through the AAGL. To complete the application process, please visit the AAGL website.
The University of Michigan offers highly competitive salaries and generous benefits to our fellows and advanced trainees. Trainee salary will be commensurate with that of a House Officer at an equivalent level of training based on the HOA contract.
Current advanced trainees in Minimally Invasive Gynecologic Surgery are developing skills to succeed as clinically skilled, compassionate obstetrician-gynecologists. We emphasize teamwork, excellence, and leadership.
- Katharine Ciesielski, MD
2022-2024 Minimally Invasive Gynecologic Surgery Fellow
Next Step: Joining the MIGS faculty at Cedars Sinai - Alexandra Foxx, MD
2021-2023 Minimally Invasive Surgery Advanced Trainee
Next Steps: Assistant Professor, University of Rochester, Rochester, NY - Gabrielle Whitmore, MD
2020 – 2022 Minimally Invasive Surgery Fellow
Next Steps: University of Colorado
- Jennifer Travieso, MD
2019 – 2021 Minimally Invasive Surgery Fellow
Next Steps: University of Texas at Austin - Kendall Griffith, MD
2018 – 2020 Minimally Invasive Surgery Advanced Trainee
Next Steps: Michigan Medicine

Chair, Department of Obstetrics and Gynecology
Professor of Obstetrics and Gynecology
Professor of Urology
Assistant Medical Director
Minimally Invasive Gynecologic Surgery Advanced Training Program
Chelsea Gynecology
Program Associate
Minimally Invasive Gynecologic Surgery Advanced Training Program
Chelsea Gynecology
Service Chief
Clerkship Assistant


Nationally-recognized physicians provide patients with a full spectrum of pregnancy and childbirth care, as well as gynecologic care before and after pregnancy. For high-risk pregnancies, U-M Medical School’s Fetal Diagnosis and Treatment Center offers comprehensive fetal services, utilizing the latest technological advances in diagnostics, minimally invasive surgeries and open surgeries.

We find a new reason to love Ann Arbor nearly every day — year-round outdoor activities, cultural experiences, a growing food scene, and a welcoming, family-friendly atmosphere are just a few that come to mind. Explore all that Ann Arbor and our surrounding communities have to offer.