At the U-M Medical School Section of Thoracic Surgery, we apply a multidisciplinary approach to research that spans basic science, translational, health disparities and outcomes.
We use what we learn to improve the lives of patients through new technologies, new care paradigms, and new understanding of the underpinnings of devastating diseases like esophageal and lung cancer.
We're paving the way for innovation in thoracic surgery, translating biomedical breakthroughs into practical applications. Our discoveries improve the lives of people in our local, national and global communities.
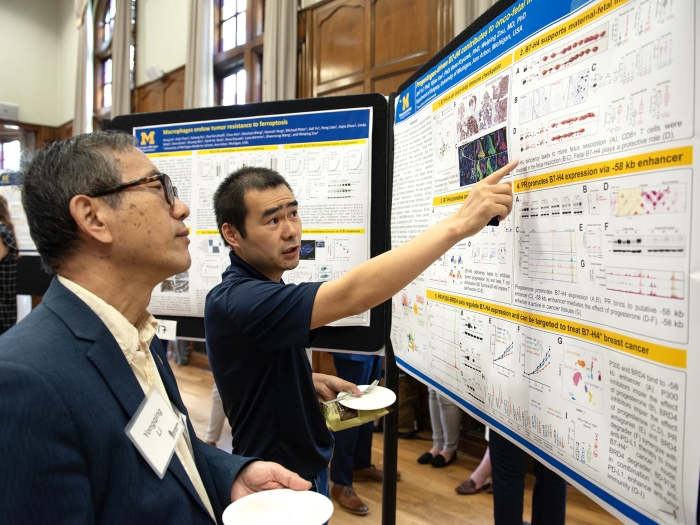
Our Thoracic Surgery Cancer Biology Lab - involving many surgeons - explores innovative developments in this area of research. With more than 25 years invested into research of esophageal and lung cancers, we’re able to investigate human disease not just through models but through the study of tissue samples.
Our tumor bank — one of the largest genetic databases of esophageal and lung cancers in the world — informs our insights into the mechanics of cancer progression so that we can ultimately develop better screening tools. We are collaborating with our Chemical Engineers to develop an early circulating tumor cell test for patients with early stage lung cancers.
We seek to be the first team to develop a powerful diagnostic test for esophageal cancer in the same way that routine colonoscopies offer the first chance to identify and even treat colon cancer at the earliest stages.
We’re one of the first institutions in the country to use the technique of ex vivo lung perfusion (i.e. “incubator in a box”) to heal damaged or deconditioned donor lungs so they can be recovered for use as transplant organs.
Currently, fewer than 20% of possible donor lungs are healthy enough to transplant due to lung bruising that occurs at the time of death. With the “lung incubator” technique, we see potential to double the number of healthy donor lungs available to waiting patients.
We’re currently one of 13 centers nationwide participating in the trial to test this technology and approach.
Performing 100 to 150 esophagectomies each year, we’re among the highest-volume programs in the country with excellent outcomes, giving us the opportunity to set the standard of care and define what the best outcomes look like for patients with esophageal cancer. Current efforts include research to understand health disparities due to race, gender and socioeconomic status. We are also evaluating new feeding paradigms to improve nutrition before and after esophagectomy. Other faculty are evaluating tumor response to chemoradiation, which occurs prior to operation. We are leaders in the state-wide and national databases on esophageal cancer outcomes that documents metrics for care and clinical quality as well.
Using the wealth of data contained within CT scans, we’ve partnered with our surgical colleagues developing the new field of analytic morphomics, which uses computer algorithms and image analysis to develop predictive models of how patients will fare after an organ transplant or esophageal cancer treatment.
By compiling and analyzing the physical variations in our patient population, we’re able to identify patients who need “prehabilitation” to improve their health before their operation. The University of Michigan Department of Surgery is the creator and leader in this new science, which is changing the way surgeons think about patient outcomes.
A simulation education effort by Dr. Mark Orringer aims to reduce leak complications associated with cervical esophagogastric anastomosis by practice and repetition. “Blunt” transhiatal esophagectomy (THE) was re-popularized in our initial Section of Thoracic Surgery report on the operation in 1978, and since then the feasibility and greater safety of a cervical esophagogastric anastomosis (CEGA) over the traditional intrathoracic esophagogastric anastomosis firmly established. While a CEGA carries a lower risk of post-esophagectomy mediastinitis, it is associated with an average reported 12-14% leak rate, and nearly 50% of such leaks ultimately result in an anastomotic stricture and a poor functional result for an operation intended to provide comfortable swallowing. A CEGA leak is at least partly technically related and theoretically reducible with simulator practice.
A novel, low-cost, medium-fidelity simulated CEGA operative site has been engineered to offer hands-on practice of a stapled side-to-side CEGA. A simulation-based curriculum in the form of a narrated video of the procedure has been developed and accompanies the simulator.
Esophageal & Lung Cancers
Our work spans from basic science research to understand the cellular and molecular events that lead to the development of esophageal and lung cancers, to improving cancer detection, to studying surgical outcomes. We are one of the few programs nationally with a high-enough case volume in surgical treatments of these cancers, so we’re able to draw on robust data and experience.
Esophageal Diseases
Rates of benign esophageal diseases, including achalasia, reflux, and hiatal hernia, are rising, with few medical treatments available to patients and little current understanding of the mechanisms of these diseases. We’re studying the outcomes for surgical treatments for esophageal diseases to improve options for patients, including examining the impact of laparoscopic techniques vs. traditional open surgery.
Extracorporeal Life Support & Lung Transplant
We’re pursuing breakthroughs in treatments for end-stage lung disease, including the development of an ex vivo lung perfusion program to heal donor organs that would not otherwise be suitable for transplant — a technique that would greatly expand the number of donor lungs available to waiting patients. We’re also an international leader in “artificial lung” research, and current projects examine how such a technology would serve as a bridge to transplant.
Health Outcomes
Our outcomes research demonstrates the power of asking patients to perform simple healthy living exercises before their surgeries, leading to better results later. We use a novel online pre-op risk assessment tool to identify patients to participate in this program, which aims to reduce surgical complications, reduce healthcare expenditures, and improve the health and outcomes of patients.
Your contribution helps us research medical breakthroughs, make medicine more inclusive and train the next generation of surgical leaders.