The U-M Medical School Section of Pediatric Surgery is one of the most established and well-funded units dedicated to discovery and education in the country.
Through inquiry and creative questioning, we seek to push current medical understanding to new realms, improving the way pediatric surgery is practiced across the profession.
Our research mission spans basic, translational, clinical outcomes, and health services domains. Resources for pediatric surgery research at U-M are broad and deep, from the Department of Surgery, ranked in the top 5 for National Institutes of Health funding, to the Institute for Healthcare Policy & Innovation, which unites and supports more than 500 researchers in efforts to improve how we deliver care.
Our current projects include development of an artificial lung and an artificial placenta; multi-institutional pediatric surgical clinical trials; organoid development using stem cells; developmental pathways of neuroblastoma; achieving autonomy in surgical education.
Our research enterprise is enriched by the connections we make across Michigan Medicine, where over 2 million patient visits a year provide rich material and inspiration for discovery, and across institutions, where we partner with colleagues around the country and the world, such as through the Midwest Pediatric Surgery Consortium, which unites the efforts of more than 10 children’s hospitals to perform multi-center clinical studies for pediatric surgical diseases.
We work with trainees at various stages of their career, from University of Michigan undergraduates in the Undergraduate Research Opportunity Program (UROP) to fellows in the Pediatric Surgery Research Fellowship, to advance the field of pediatric surgery with innovative investigations.
We’re pursuing multiple studies in this area, including clinical research on congenital diaphragmatic hernia and quality improvement work on tracheoesophageal fistula.
Through our expertise in both pediatric surgical care and intensive care, we’re uniquely positioned to understand patients’ needs in both realms. Current projects include: an FDA-funded study on the amount of fat included in IV nutrition with the goal of preventing liver damage later; as well as investigation of neonatal GI problems, abdominal wall defects, NEC, appendicitis and inflammatory bowel disease.
We partner with patients and families to change how care is provided. Through the NEC Society, we collaborated with families to incorporate the social aspects of health care that impact how patients will fare. Through the Child Health Evaluation & Research Center (CHEAR), we’re working on areas such as: projecting long-term clinical and economic outcomes; using mobile technologies for chronic disease management; and developing a national platform for sharing unscheduled pediatric care benchmarks.
We’re working to understand the pathways that lead to the development of childhood cancers, including research into possible new targets for neuroblastoma, which is responsible for up to 10 percent of all pediatric cancers.
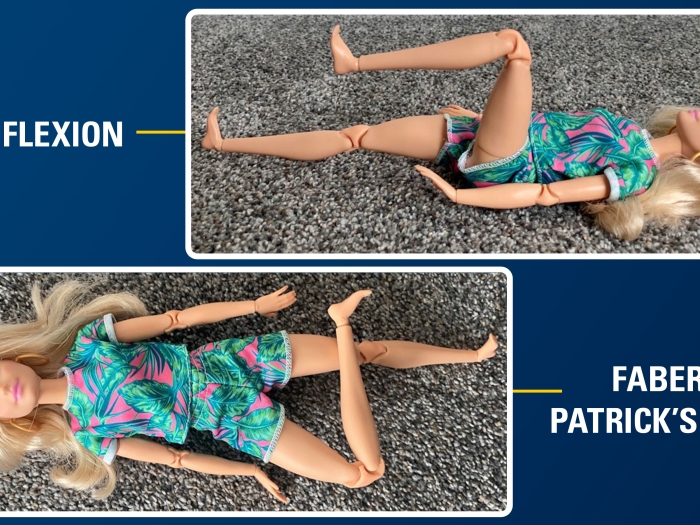
As one of the only Level 1 trauma centers in the state, we draw on our clinical experience to design interventions for trauma and injury. We set standards and educate other regional institutions on best practices, and our research focuses preventing recurrent trauma, including through substance abuse counseling for teens and a grant-funded “don’t text and drive” campaign. Our researchers use analytic morphomics to evaluate how injury impacts patients of different ages and body types to create safer car restraints. The impact of ECLS technology is also being explored in multiple faculty research initiatives, such as artificial placenta and fetal surgical interventions.
Your contribution helps us research medical breakthroughs, make medicine more inclusive and train the next generation of surgical leaders.