A new teaching tool, Radar, is helping teams improve their shared decision-making skills in educational and patient settings. Innovator Vitaliy Popov is receiving funding and support through the RISE Innovation Development Program. The project was originally funded through the Center for Interprofessional Education.
A patient is meeting with members of their health care team to discuss treatment options for managing a newly diagnosed condition. The appointment is short and a lot of new information is being shared that will impact the patient’s life. It is key that the team works well together to support the patient and to help them make a treatment decision that is right for them.
The patient is presented with two options. From a clinical perspective, option A might make the most sense to the care team. However, the patient might prefer option B, which aligns with their personal values or the impact on their quality of life.
It is important that the team and the patient arrive at a shared decision for how to move forward with the treatment. If you’re a clinician, have you ever left wondering if you and the patient are on the same page after a patient encounter?
A tool for shared-decision making
Enter Vitaliy Popov, Ph.D., assistant professor of learning health sciences in the University of Michigan Medical School. Popov developed Radar, a teaching tool used to aid in interprofessional shared decision-making (SDM).
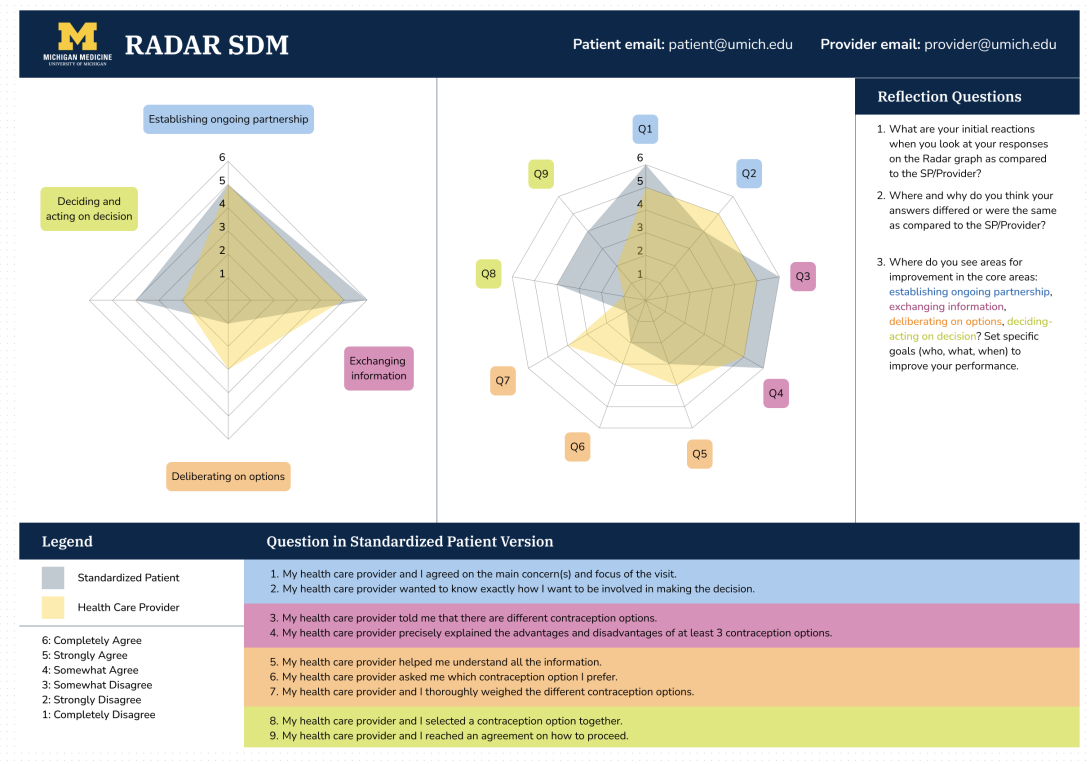
The tool borrows its name from the radar system that detects and displays objects in its vicinity. In this case, the Radar detects and highlights areas where there are misalignments or differences in how the care team and how a patient views a particular shared decision-making situation. By condensing and visualizing these perspectives into a single display, the tool allows users to quickly identify and focus on the areas where perspectives diverge or do not align. This enables them to then deliberate and work towards resolving those misalignments to reach a shared understanding and decision.
Popov is also an assistant professor of information in the School of Information and director of learning sciences and technology for the Clinical Simulation Center. Together, his roles combine research with teaching and service, an ideal combination for developing a shared decision-making tool that can be used in both education and patient settings.
In order to develop their SDM skills, health care professionals need frequent, realistic training opportunities that offer meaningful feedback.
“Right now in medical education, there is not a systematic way to approach shared decision-making for professional teams through a curriculum,” shared Popov.
“Students tend to learn this in a more spontaneous way, so my hope is that Radar can make this training more systematic and data-informed.”
Radar works by mapping four constructs of SDM — establishing an ongoing partnership, exchanging information, deliberating options, and deciding and acting on a decision — through a series of nine questions.
Members of the health care team and the patient complete these questions via a web-based survey after an appointment. Once everyone has answered the questions, the provider can access a real-time visualization that includes all perspectives. This helps identify any areas of disagreement within the health care team that should be discussed further, and also helps them understand whether the patient is fully understanding the information that was discussed.
“Sometimes a patient may need more information or additional time to digest their options. The tool helps bring these items to the surface so the care team can adjust the treatment plan rather than closing the door,” explained Popov.
Radar can be customized to meet the needs of various teams in different settings. For example, larger teams may need more questions to meet the needs of multiple stakeholders.
To date, Radar has been implemented in three settings at Michigan Medicine — a standardized patient simulation on contraception counseling for medical students, a simulation-based training for dental students on chronic obstructive pulmonary disease and angina, and among the prostate cancer center team at the University of Michigan Rogel Cancer Center.
The standardized patient simulation is an educational setting where medical students work with trained individuals to portray a specific patient case. In this setting, students and the standardized patients answer the SDM questions and use the results during debriefing sessions to reflect on areas of improvement. This allows them to practice their communication skills in a safe environment.
So far over 180 medical students have used the tool as part of their curriculum.
“I thought this tool was super helpful and gave me concrete things to reflect on, and having this data to go over in the presence of someone to give me real-time feedback made for excellent learning,” said a medical student.
Dental students utilized the tool as part of a combined simulation for those in respiratory and cardiovascular system courses. Over 240 second year dental students participated. Here Radar was able to help identify educational targets for improvement related to items such as establishing credibility, providing options for patients linked to a rationale and information retrieval when deliberating choices.
The tool can also be used outside of an educational setting to help care teams and their patients with shared decision making in clinical settings.
The prostate cancer center team has used Radar with seven providers and 60 patients so far and is looking to scale it further. In this setting, the tool acts as a quality control mechanism where providers can identify points of misalignment with patients after a visit and make a follow-up call to help resolve any misunderstandings or offer support. Here, the stakes are much higher as the team is making life or death decisions surrounding treatment plans.
As Popov continued to refine Radar and implement the tool in additional settings, he engaged Michigan Medicine’s RISE team for additional support.
Where RISE is helping
Popov participated in the RISE Innovation Development Program, which supports new ideas in health sciences education innovation through a series of workshops and individual support.
“I think it’s a very well-rounded program that brings together the spirit of entrepreneurship and innovation in service to education.”
Coming from a research background, Popov found the program useful for developing skills related to pitching the tool to clinicians and getting their buy-in. RISE taught him to focus on the benefits of the tool and how it can help with shared decision-making in their specific areas.
“As a trained academic, I’m focused on the research questions. Without RISE, I may have lost potential users — providers, trainees, instructors — who couldn’t see the relevance to their specific specialties.”
Popov also appreciated the feedback he received from his fellow RISE Cohort members.
“Not only are they people who can provide high quality feedback on my innovation, but they are all passionate educators and clinicians,” Popov shared. “It was helpful to hear how others work through the process of developing their projects.”
Scaling Radar
Popov hopes to continue to scale Radar to help with shared decision-making in both educational and clinical settings across Michigan Medicine.
For learners, having more intentional and frequent training opportunities can help them be more successful when communicating with their teammates and with patients. Creating a better framework for teamwork means better alignment and less frustration for the entire team, leading to better treatments for patients.
Those wishing to implement Radar to help with shared decision-making should contact Popov for a consultation. The tool can be customized to meet a team’s specific needs.
“Hopefully it can make a difference in patients’ lives and make the life of the care provider a bit easier.”
Please contact Vitaliy Popov ([email protected]) if you are interested in implementing Radar to help with shared decision-making in your area.
To stay informed about RISE opportunities and education innovations happening at Michigan Medicine, join our community.
Photo credits: Camren Clouthier
Graphic: Vitaliy Popov

Assistant Professor