Certain nighttime habits can either help or hurt sleep issues in young children
5:00 AM
Author |

Many bedtime battles stem from children’s after dark worries, suggests a national poll.
And while most families have bedtime rituals to help their little ones ease into nighttime, many also rely on strategies that may increase sleep challenges long term, according to the University of Michigan Health C.S. Mott Children’s Hospital National Poll on Children’s Health.
Overall, one in four parents describe getting their young child to bed as difficult – and these parents are less likely to have a bedtime routine, more likely to leave on a video or TV show, and more likely to stay with their child until they’re asleep.
"Our report reinforces the common struggle of getting young children to sleep. When this transition to bedtime becomes a nightly conflict, some parents may fall into habits that work in the moment but could set them up for more sleep issues down the road,” said Mott Poll co-director Sarah Clark, M.P.H.
“Establishing a consistent bedtime routine is crucial. When children don’t get enough rest, it can impact their physical development, emotional regulation and behavior.”
Nearly one in five parents say they have given their kids melatonin to help with sleep while a third stay in the room until their child completely dozes off, according to the nationally representative poll that includes responses from 781 parents of children ages one to six surveyed in February.
Nighttime worries interfere with sleep
Parents share common reasons behind bedtime struggles, with nearly a quarter saying their child’s sleep is often or occasionally delayed due to being worried or anxious.
A particular challenge, parents say, is when children don’t stay asleep.
More than a third of parents say their child wakes up upset or crying, with more than 40% saying their child moves to their parents’ bed and about 30% saying children insist that the parent sleep in their room.
“Many young children go through stages when they become scared of the dark or worry that something bad might happen, causing them to delay bedtime or become distressed by parents leaving the room. Bad dreams or being awakened in the middle of the night can also disrupt sleep,” Clark said.
“Although this is a normal part of a child’s development, it can be frustrating when parents already feel tired themselves at the end of the day. Parents should find a balance between offering reassurance and comfort while maintaining some boundaries that help ensure everyone – both kids and adults – get adequate sleep.”
Below are more findings from the report, plus Clark’s recommendations for helping young children fall and stay asleep.
Stick to a regular bedtime routine
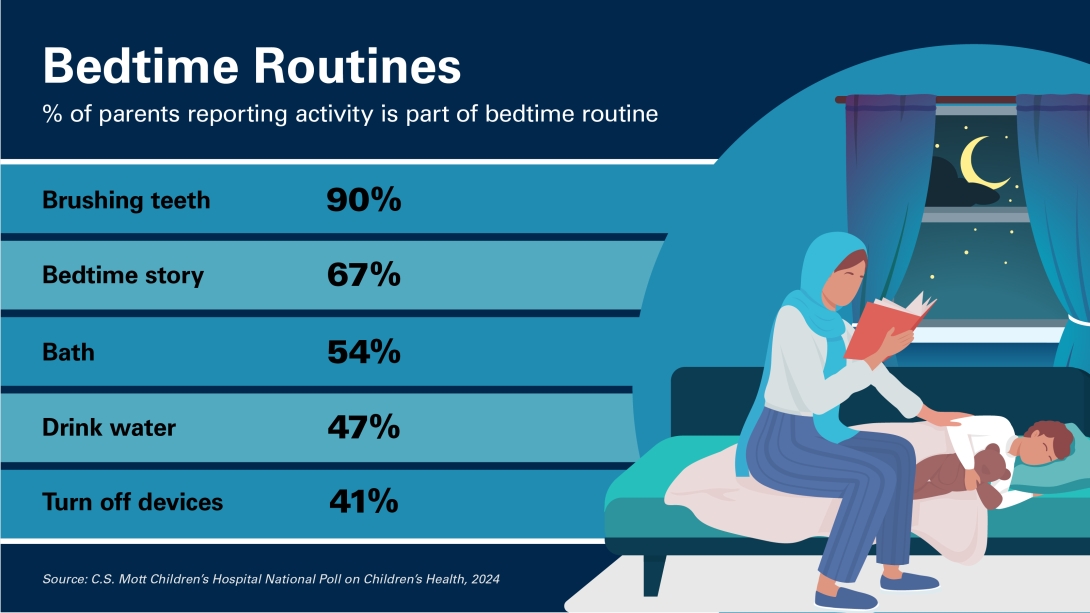
Most parents polled report having a bedtime routine for their child, often including brushing teeth, reading bedtime stories and/or bathing.
Less than half also say their child has a drink of water or snack, turns off devices, prays and talks about their day.
Other bedtime habits include holding a blanket or stuffed animal or sucking a pacifier or fingers.
Our report reinforces the common struggle of getting young children to sleep. When this transition to bedtime becomes a nightly conflict, some parents may fall into habits that work in the moment but could set them up for more sleep issues down the road.”
- Sarah Clark, M.P.H.
Not only does having a consistent bedtime routine help make the nighttime transition smoother, Clark says, it also provides one-on-one time, allowing the child to get their parent’s full attention.
“A predictable bedtime routine provides a sense of security and comfort and signals to the child that it’s time to slow down,” she said.
“Knowing what to expect next can reduce anxiety and help children feel safe and relaxed. Having this dedicated time with parents also promotes bonding and emotional connection, creating positive associations with bedtime.”
Nearly two-thirds of parents also said children staying up to play was a major factor in delaying sleep, highlighting the need to wind down at least an hour before bed.
Promote an environment conducive to sleep
A little less than half of parents polled say their child sleeps in their own bedroom while less than a quarter share a bedroom with siblings.
One in 10 kids spend part the night in their own bedroom and part of the night with parents.
More than two-fifths of parents polled said noise from other rooms interfered with their child’s sleep.
“The sleep environment can have a major effect on a child’s sleep quality, including getting to sleep and staying asleep through the night,” Clark said.
“When possible, children should have their own bed in a room that is quiet, without a lot of noise from other family members.”
Many parents polled also use a nightlight or crack the bedroom door so the child isn’t in complete darkness, Clark says, but parents should make sure the light does not shine directly at the child’s face.
Some parents also play calming music or stories to help their child go to sleep, while others use a white noise machine or app.
However, Clark cautions to keep white noise machines at no more than 50 decibels and be placed at least seven feet from the child’s bed to prevent unintended damage to the child’s hearing.
Talk to a doctor before using aids like melatonin
Many types of melatonin products are advertised as being appropriate for children but these products have not undergone rigorous testing for safety and effectiveness, and their side effects and long term impact on a child’s growth and development are unknown, Clark says.
“Although melatonin is a natural hormone that regulates sleep-wake cycles and may be fine to use occasionally, parents shouldn’t rely on it as a primary sleep aid,” Clark said.
“Parents who are considering giving melatonin to their young child should consult with their pediatrician to discuss options and rule out other causes of sleep problems first.”
If using melatonin, parents should also start with the lowest dose possible.
In addition, it is important to keep electronics such as tablets or televisions out of children’s bedroom, as the blue light emitted by many of these screens interferes with the natural production of melatonin.
Offer comfort but enforce boundaries
Parents can help ease little ones’ anxiety by allowing extra time to let them talk about their day, which might draw out specific worries and give parents a chance to provide compassion and reassurance, Clark said.
Rather than remaining in the room, parents can also offer to check on the child every few minutes, which acknowledges the child’s fears and offers a reassuring presence, but still maintains a calm sleep environment and promotes sleep independence.
“Families can incorporate comforting rituals to help transform nighttime fears into a calming experience,” Clark said.
Have a consistent approach when children wake up in the night
Some children are prone to vivid dreams or nightmares and may have difficulty getting back to sleep.
Parents should decide on their approach to this situation and stick with it, Clark says, whether it’s taking the child back to bed or allowing them to stay in the parents’ room.
“Being consistent in carrying out that approach will help the child adjust and be more likely to return to sleep,” Clark said.
Ease into changes in sleep patterns, such as dropping naps
For young children, a major sleep-related transition is discontinuing daytime naps. In general, children ages one to two should get 11-14 hours of sleep with naps while the amount of recommended sleep decreases slightly from ages three to six.
If children are taking longer to fall asleep at nap time, resisting naps or suddenly having difficulty falling asleep at night or waking up earlier than usual in the morning, it may be time to drop the nap, Clark says.
“Parents may need to adjust sleep routines gradually to transition to changes to a child’s sleep patterns,” Clark said.
Other changes that can affect a child’s sleep include transitioning from a crib to a toddler bed, starting school, having a change in their daytime routine, or being outdoors for longer than usual.
Sign up for Health Lab newsletters today. Get medical tips from top experts and learn about new scientific discoveries every week by subscribing to Health Lab’s two newsletters, Health & Wellness and Research & Innovation.
Sign up for the Health Lab Podcast: Add us on Spotify, Apple Podcasts or wherever you get you listen to your favorite shows.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine

Research Scientist
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!