The ability to accurately detect where X-rays land and in what dose could reduce the collateral damage from radiation therapy.
1:14 PM
Author |
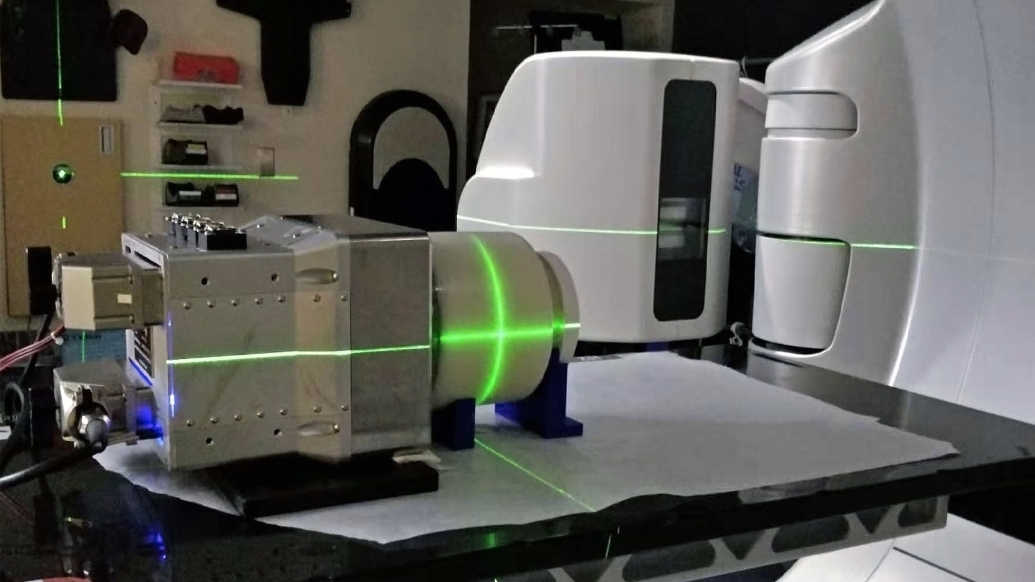
Radiation, used to treat half of all cancer patients, can be measured during treatment for the first time with precise 3D imaging developed at the University of Michigan.
By capturing and amplifying tiny sound waves created when X-rays heat tissues in the body, medical professionals can map the radiation dose within the body, giving them new data to guide treatments in real time. It’s a first-of-its-kind view of an interaction doctors have previously been unable to “see.”
“Once you start delivering radiation, the body is pretty much a black box,” said Xueding Wang, Ph.D., professor of radiology at the University of Michigan Medical School, the Jonathan Rubin Collegiate Professor of Biomedical Engineering at U-M and corresponding author of the study in Nature Biotechnology. He also leads U-M’s Optical Imaging Laboratory.
“We don’t know exactly where the X-rays are hitting inside the body, and we don’t know how much radiation we’re delivering to the target. And each body is different, so making predictions for both aspects is tricky.”
Radiation is used in treatment for hundreds of thousands of cancer patients each year, bombarding an area of the body with high energy waves and particles, usually X-rays. The radiation can kill cancer cells outright or damage them so that they can’t spread.
These benefits are undermined by a lack of precision, as radiation treatment often kills and damages healthy cells in the areas surrounding a tumor. It can also raise the risk of developing new cancers.
SEE ALSO: Side effects of radiation therapy reduced when computer optimizes treatment, study finds
With real-time 3D imaging, doctors can more accurately direct the radiation toward cancerous cells and limit the exposure of adjacent tissues. To do that, they simply need to “listen.”
When X-rays are absorbed by tissues in the body, they are turned into thermal energy. That heating causes the tissue to expand rapidly, and that expansion creates a sound wave.
The acoustic wave is weak and usually undetectable by typical ultrasound technology. U-M’s new ionizing radiation acoustic imaging system detects the wave with an array of ultrasonic transducers positioned on the patient’s side. The signal is amplified and then transferred into an ultrasound device for image reconstruction.
With the images in-hand, an oncology clinic can alter the level or trajectory of radiation during the process to ensure safer and more effective treatments.
“In the future, we could use the imaging information to compensate for uncertainties that arise from positioning, organ motion and anatomical variation during radiation therapy,” said Wei Zhang, a research investigator in biomedical engineering and a co-first author of the study. “That would allow us to deliver the dose to the cancer tumor with pinpoint accuracy.”
In future applications, this technology can be used to personalize and adapt each radiation treatment to assure normal tissues are kept to a safe dose and that the tumor receives the dose intended.
Another benefit of U-M’s technology is it can be easily added to current radiation therapy equipment without drastically changing the processes that clinicians are used to.
“In future applications, this technology can be used to personalize and adapt each radiation treatment to assure normal tissues are kept to a safe dose and that the tumor receives the dose intended,” said Kyle Cuneo, M.D., clinical associate professor of radiation oncology at the U-M Medical School. “This technology would be especially beneficial in situations where the target is adjacent to radiation sensitive organs such as the small bowel or stomach.”
Additional authors include Ibrahim Oraiqat, Christopher J. Tichacek and Eduardo G. Moros of the Moffitt Cancer Cancer and Issam El Naqa, Dale Litzenberg, Kai-Wei Chang, Scott Hadley, Noora Ba Sunbul, Martha M. Matuszak and Paul L. Carson of U-M.
Funding: National Cancer Institute and the Michigan Institute for Clinical and Health Research
Issam El Naqa, Xueding Wang, Paul L. Carson, Kai-Wei Chang, Wei Zhang and Ibrahim Oraiqat have applied for a patent on this technology.
Paper cited: “Real-time, volumetric imaging of radiation dose delivery deep into the liver during cancer treatment,” Nature Biotechnology. DOI: 10.1038/s41587-022-01593-8
Live your healthiest life: Get tips from top experts weekly. Subscribe to the Michigan Health blog newsletter
Headlines from the frontlines: The power of scientific discovery harnessed and delivered to your inbox every week. Subscribe to the Michigan Health Lab blog newsletter
Like Podcasts? Add the Michigan Medicine News Break on Spotify, Apple Podcasts or anywhere you listen to podcasts.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!