It’s a major surgery, but can make a huge difference in a woman’s quality of life
5:00 AM
Author |

While the definition of a hysterectomy is the surgical removal of the uterus, to many it means much more than that. It’s hope. It’s a cure. It’s life changing.
“A hysterectomy is the maximum therapy for a uterine problem,” said Bethany Skinner, M.D., a gynecologic surgeon who specializes in minimally invasive surgery at University of Michigan Health Von Voigtlander Women’s Hospital. “If you experience chronic abnormal bleeding or have fibroids, this may be the answer for you. It’s the definitive management for those problems.”
The most common conditions a hysterectomy treats include:
- Uterine fibroids – benign, often painful growths that can cause heavy bleeding
- Uterine prolapse – weak tissue supporting the uterus that slips into the vagina
- Endometriosis – tissue, like that of the lining of the uterus, that grows outside of the uterus
- Adenomyosis – thickening of the uterus
- Cancer or precancer of the uterus, cervix, ovaries or endometrium (the lining of the uterus)
- Heavy or unusual vaginal bleeding
What is a hysterectomy?
Hysterectomies are the second most performed surgical procedure for women in the United States (first being cesarean section).
About 600,000 people seek one annually and, by age 60, more than one-third of all women have had a hysterectomy, according to the National Women’s Health Network.
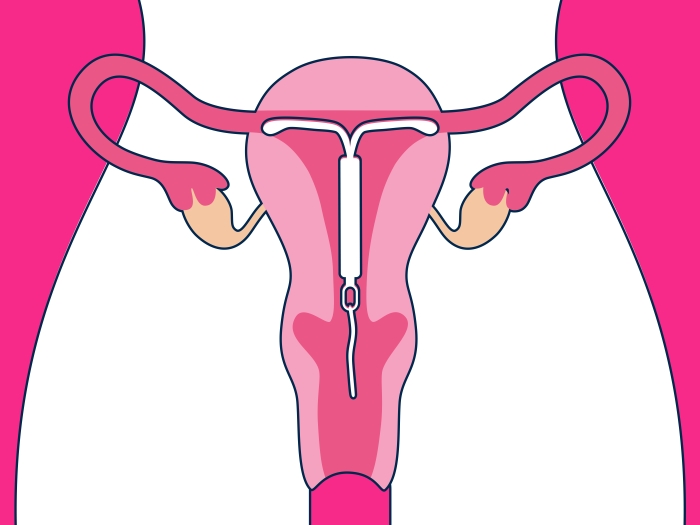
The removal of your uterus stops menstrual periods and ends your ability to become pregnant. Because of this, there are some nonsurgical methods doctors try to use first to treat these conditions.
“When a patient comes to see me, we discuss all the options,” Skinner said. “They come with a list of questions and, during that discussion, it’s important to keep an open mind about the pros and cons of this major surgery compared to the pros and cons of the other treatment options.”
Here’s what you need to know before talking to your doctor about having this often-elective, but indicated, surgery.
Types of hysterectomies
There are four main types of hysterectomies your doctor may discuss with you, and the one you have will be dependent on your condition and consultation with your physician:
- Partial (or subtotal or supracervical) hysterectomy – removes the upper region of the uterus. The cervix remains and the ovaries may or may not be removed.
- Total hysterectomy – the most common type, removes the entire uterus and the cervix. The fallopian tubes and ovaries may or may not be removed.
- Radical hysterectomy – removes all of the uterus, cervix and tissue on the sides of the cervix and the upper part of the vagina. This procedure is often used to treat certain cancers, like cervical cancer. The fallopian tubes and ovaries may or not be removed.
- Hysterectomy with bilateral salpingo-oophorectomy – removes the uterus, cervix, fallopian tubes and ovaries.
There are also four different ways your surgeon can perform a hysterectomy. This includes:
- Vaginal – when the surgeon removes the uterus through a small cut in the vaginal canal. This method requires less healing time and is considered the least invasive.
- Abdominal – also known as an open incision, the cut is in the lower abdominal area – either along the bikini line or vertical – and is the method used when removing a very large uterus or for certain types of cancer. It’s the most common type.
- Laparoscopic – sometimes called keyhole surgery, this involves a laparoscope – a lighted tube with a small camera – to remove the uterus through small cuts either in the abdomen or vagina.
- Robotic – using a robotic arm, a laparoscope, and three to five incisions near the belly button, a doctor removes the uterus while looking at a video screen rather than at the bedside, standing over the patient.
Do you have a say in which surgical method is used for your hysterectomy?
Often, yes, but the minimally invasive approach is preferred when feasible because of lower risk and quicker recovery times, Skinner said.
When a patient comes to see me, we discuss all the options. During that discussion, it’s important to keep an open mind about the pros and cons of this major surgery compared to the pros and cons of the other treatment options.” –
A laparoscopic or a vaginal hysterectomy can also shave two weeks off your recovery time. The recovery from an abdominal hysterectomy can take about six to eight weeks, but the smaller the incision, the quicker the recovery.
Unfortunately, your anatomy or health history won’t always allow for a laparoscopic or vaginal procedure, Skinner explained.
Laparoscopic hysterectomies, for instance, aren’t done on those with certain lung or heart issues. That’s because the operating table needs to be tilted, resulting in your head down and feet high in the air, causing blood to rush to your brain and put pressure on the heart and lungs.
If you have a larger uterus, your doctor may need to perform abdominal surgery, and the same applies for some women with cancer, Skinner said.
And, although it doesn’t exclude you from having a laparoscopic surgery, she added, prior multiple c-sections may mean that a vaginal hysterectomy isn’t the best option for you.
The benefits of a hysterectomy
Skinner recognizes the psychological impact hysterectomies have on some patients, since it ends their ability to birth children.
On the other hand, there are many others who report feeling like they get to live again because of how the procedure improves their quality of life.
Heavy bleeding and pain can keep some patients homebound or alter their way of living. But many report that stopping the bleeding has changed their lives for the better.
“For some women, heavy bleeding and pressure from fibroids inhibited their sex lives but, after surgery, they are having happy, healthy sex lives,” Skinner explained.
Other women report less pressure on their bladder, so they can hold their urine longer, which helps them sleep better since they’re not constantly getting up at night to visit the bathroom. And better sleep makes every day better.
“A hysterectomy can help many women improve their lives,” she says

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!