Around 10,000 Americans each year are diagnosed with glioblastoma
9:01 AM
Author |

After an awake surgery to remove a cancerous brain tumor, a Michigan man is living “more deliberately” than ever — officiating a high school wrestling state championship and participating in research for a potential cure.
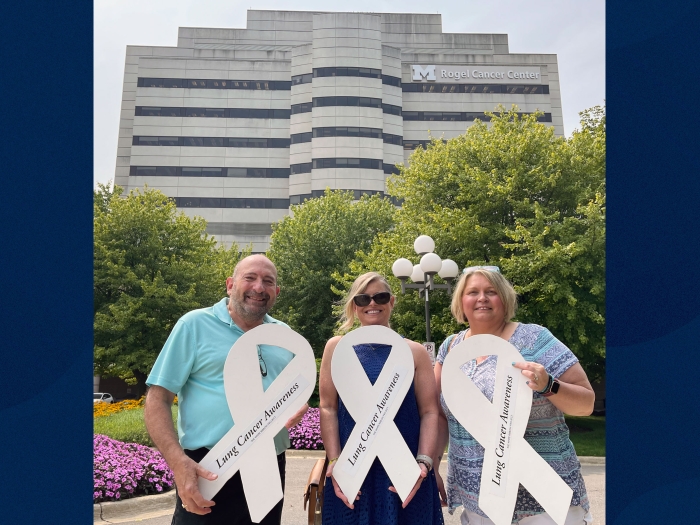
Phil Shannon, 52, returned to the mat in March 2023, two years after being diagnosed with glioblastoma, the most aggressive and fast-growing tumor that forms in the brain.
“I have gone back to living my life again as close to 100% as I could ever dream of being,” said Shannon, a former process engineer from Dearborn Heights, Mich.
“I don’t think about statistics as much as I once did. I am living within moments with new hope.”
‘Started to make preparations’
Shannon’s diagnosis unfurled slowly. In early 2020, his wife, Emma Shannon, noticed that Phil would misgender their dog. He began mixing up simple, multi-syllable words and became more fatigued.
At their family cottage in northern Michigan later that year, Phil Shannon spent the entire trip on the couch. Emma Shannon says everything cascaded very quickly after that.
“Our primary doctor told us to drive to the emergency room right away; he had seen something on the scan,” she said.
“Our daughter Mindy, who is a nurse practitioner at University of Michigan Health, drove him there.”
Imaging showed a glioblastoma, a diagnosis more than 10,000 Americans each receive year, in Phil Shannon’s language-dominant cortex. Wajd Al-Holou, M.D., a neurosurgeon at U-M Health, told Shannon that an awake brain surgery was needed to remove as much of the tumor as possible while maintaining his normal brain function.
“During an awake surgery, we expose the brain and identify the location of important areas that control language function, for example,” Al-Holou said.
SEE ALSO: Outsmarting brain cancer (michiganmedicine.org)
“This is done by stimulating various brain regions while asking the patient to name objects and answer questions. When we correctly stimulate a certain area, the patient will not be able to respond. This allows us to mark the critical parts of the brain we need to save, and the parts of the tumor that we can resect to ensure that a patient does not have language deficits after the procedure.”
The average survival rate for patients with this malignant tumor is poor. It can range from six to nine months for patients who don’t have surgery and can potentially increase to 18 months or longer for those who have surgery to remove it.
Al-Holou was as honest as possible with Shannon: the more of the tumor they could remove, the better chance of a positive outcome. They scheduled the surgery for January 28, 2021.
“Emma and I are both logical people,” Phil Shannon said.
“We started to make preparations; we made sure the family would be taken care of. Throughout all of this, Dr. Al-Holou was very comforting. Even during the surgery, he was working on my brain while I was awake, and he made it feel like a walk in the park.”
The awake surgery tumor resection
University of Michigan Health is one of few programs in the nation that offer a comprehensive awake brain surgery with a multidisciplinary team, which includes a neurosurgeon, neurologist, anesthesiologist, certified registered nurse anesthetist, speech language pathologist and operating room nurse and scrub technician.
During the procedure, the neurosurgical team identified Phil Shannon’s language sites immediately behind the tumor. This meant that Al-Holou was able to dissect the tumor away from the language sites while the speech pathologist actively tested Phil Shannon’s language to ensure it remained functional. Through the mapping and resection process, Al-Holou says they were able to safely remove the entire tumor.
“During the removal, we could not identify any more of the tumor,” he said.
“This was the outcome we hoped for going into the procedure. In addition, because our team is working to understand why glioblastomas are so difficult to treat, we were also able to save a part of Mr. Shannon’s tumor for this very important research.”
SEE ALSO: Using neuropsychology to heal from cancer treatment | Michigan Medicine
Right when Phil Shannon woke up, he found strength to walk the halls of his hospital floor. He began chemotherapy and radiation not long after the procedure.
“He did OK for about five weeks,” Emma Shannon said.
“But one day he had a seizure at the house. His mouth was moving, but he couldn’t speak. He went back to U-M, and the seizure lasted for almost a week.”
For some patients with gliomas, irritation from the tumor itself can cause a seizure. Radiation can trigger seizures as well. Neurologists and neurointensivists managed Shannon’s condition at U-M Health for three weeks.
Research, hope and perspective
When he woke in the hospital for a second time, Shannon developed newfound faith.
“In the neuro ICU, I met an employee named Rob who talked and prayed with me,” he said.
“Rob said one thing that turned my life around. ‘You’re not going to try; you are going to do this.’ Every day moving forward, I live this way. And I’m thankful that he shook me back to reality.”

That mentality has defined Shannon’s post-operative life. He began riding his bike more often and returned to his passion of officiating youth wrestling matches. He and Emma Shannon “don’t worry about statistics and what-ifs” that “only steal time”.
In Feb. 2023, imaging uncovered two new spots on his brain. Shannon’s care team set up another round of radiation, and he enrolled in a clinical trial, developed through research done at U-M, that will test whether the drug mycophenolate mofetil will achieve active concentration in the brains of glioblastoma patients and if it will improve the response of these tumors to radiation.
The trial is run through a specialized, multidisciplinary brain tumor clinic (Michigan Medicine Multidisciplinary Brain Tumor Clinic, or M3BTC for short) developed by Al-Holou and his colleagues in radiation oncology and neuro-oncology.
“Time is precious, and I live much more deliberately now,” Phil Shannon said.
“This trial is not just about me. Win or fail, and I expect to win, I want to give hope to people who need options to move them away from being that statistic. The only way they will be able to find new ways to deal with this condition is by people stepping up for others.”

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!