And the development of a new slow-release drug seeks to target them
12:53 PM
Author |

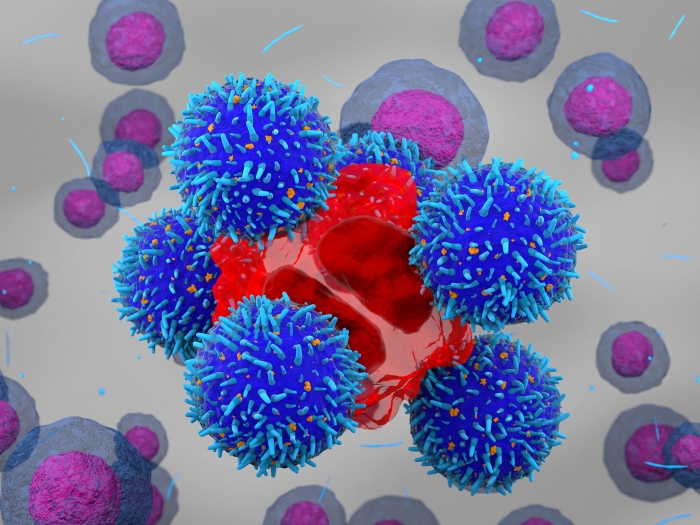
A Michigan Medicine study has identified a new potential target for treating osteoarthritis – a debilitating joint disease that affects over 31 million Americans and is a leading cause of disability worldwide.
A team of researchers led by Tristan Maerz, Ph.D., a biomedical engineer and assistant professor in the Department of Orthopaedic Surgery at Michigan Medicine has uncovered previously unknown cell types in the joint that emerge after an injury and drive the onset of osteoarthritis.
Clinically, osteoarthritis presents as a very complex disease, with patients suffering from joint stiffness, reduced mobility and function, and most notably, persistent pain.
Osteoarthritis patients commonly live with this condition for multiple decades, and no treatments have been developed that can stop or reverse the disease. The condition can occur with age or be sparked by a joint injury and is typically managed with pain relief and end-stage joint replacement.
The study “Synovial fibroblasts assume distinct functional identities and secrete R-spondin 2 in osteoarthritis” published in the Annals of the Rheumatic Diseases examined the cellular and molecular events during the onset of post-traumatic osteoarthritis in joints.
“We identified cell types that emerge in the joint after trauma, such as an ACL injury, and we can now associate these cells with the disease process,” Maerz said. “This allows us to view them as a treatment target for this devastating disease.”
By employing a cutting-edge gene sequencing technology called single-cell RNA-sequencing, Maerz and his team were able to uncover these previously uncharacterized cells that emerge in the joint after injury.
The study also described the biological processes that may activate these cells, which offers compelling new targets for an effective treatment.
“Interestingly, these cells are not found in healthy joints, and we have to understand exactly what causes them to appear and how they may cause osteoarthritis,” said Alex Knights, Ph.D., a senior post-doctoral researcher in the Maerz Laboratory, who was instrumental in uncovering and describing these cells and their biology.
Now, having identified several cell types that may be responsible for causing the disease, the Maerz Laboratory are hopeful that targeting them may be an effective osteoarthritis treatment.
“This research will further our understanding of the ways that osteoarthritis progresses, particularly after an injury to the knee,” said Elizabeth Dailey, M.D., an orthopedic surgeon treating end-stage osteoarthritis and joint replacement specialist at University of Michigan Health who is working together with Maerz and his team.
Maerz and his team are now working with biomedical specialists to develop new drug delivery systems that can be injected into joints in the aftermath of a traumatic injury to slow down or ideally halt the development of osteoarthritis.
This work will be done alongside Craig Duvall, Ph.D., a drug delivery and biomaterials engineering expert from Vanderbilt University, to create a slow-release drug to block the disease before it has a chance to take hold following joint trauma.
“This has the potential to yield a single long-lasting treatment which is necessary for patient compliance in a chronic disease like osteoarthritis. Local delivery also minimizes the possibility for side effects due to drug exposure in other tissues and organs, and it maximizes the drug benefit at the targeted disease site,” Duvall stated.
The Maerz Laboratory has been awarded a $2.5 million grant by the National Institute of Arthritis and Musculoskeletal and Skin Diseases to develop and test a biomaterial-based drug delivery system to treat osteoarthritis.
“This new study and the federal funding are a large step forward for osteoarthritis research on campus and across the country,” stated Kurt Hankenson, D.V.M., Ph.D., a senior colleague of the Maerz laboratory and the associate chair for research in the Department of Orthopaedic Surgery.
“We work closely with our surgeon colleagues to understand the clinical relevance of our laboratory research to maximize its potential impact on clinical care, which is our ultimate objective.”
This work will also seek to understand how a certain molecular signaling pathway, specifically Wnt signaling, is involved in the early activation of joint cells after injury.
“For us to be able to develop a treatment that can be given immediately after a joint injury to block this disease process gives hope for the osteoarthritis patient,” Maerz said.
Live your healthiest life: Get tips from top experts weekly. Subscribe to the Michigan Health blog newsletter
Headlines from the frontlines: The power of scientific discovery harnessed and delivered to your inbox every week. Subscribe to the Michigan Health Lab blog newsletter
Like Podcasts? Add the Michigan Medicine News Break on Spotify, Apple Podcasts or anywhere you listen to podcasts.
Paper cited: “Synovial fibroblasts assume distinct functional identities and secrete R-spondin 2 in osteoarthritis,” Annals of the Rheumatic Diseases. DOI: 10.1136/ard-2022-222773

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!