Harnessing a patient’s immune system to attack cancer proves effective for certain cancer types
5:00 AM
Author |

Kat Forsythe was on her honeymoon in northern California with her second husband, Dave “Lars” Gunstrom, when she started to experience frequent nausea.
Whenever she ate, her stomach cramped. By the end of the trip, her diet had become applesauce and vegetable soup.
Upon Kat’s return home to Dexter, Mich., she visited her primary care doctor at Michigan Medicine, Juana Nicoll Capizzano, M.D. Kat’s colonoscopy from two and a half years before had come back clean, but Capizzano ordered a new colonoscopy after considering her symptoms.
The colonoscopy came back positive for stage 4 colon cancer. Tumors had spread from her transverse colon to her peritoneum, liver and lymph nodes, with concern about nodules in her lungs.
“I was blown out of the water. My eldest daughter Kate and my husband Lars were in the examination room with me when I heard the news. It was very difficult,” Kat said.
Just over a year after her diagnosis, Kat is in full remission thanks to a new type of cancer treatment called immunotherapy.
The future of cancer treatment
After her diagnosis, Kat sat down with John Christopher Krauss, M.D., medical oncologist at the University of Michigan Health Rogel Cancer Center, to discuss treatment options.
Given her tumor type, he recommended immunotherapy as the path forward.
Pathology results characterized Kat’s tumor with high microsatellite instability, meaning the cancer cells are prone to genetic mutations as they lose the ability to fix DNA errors.
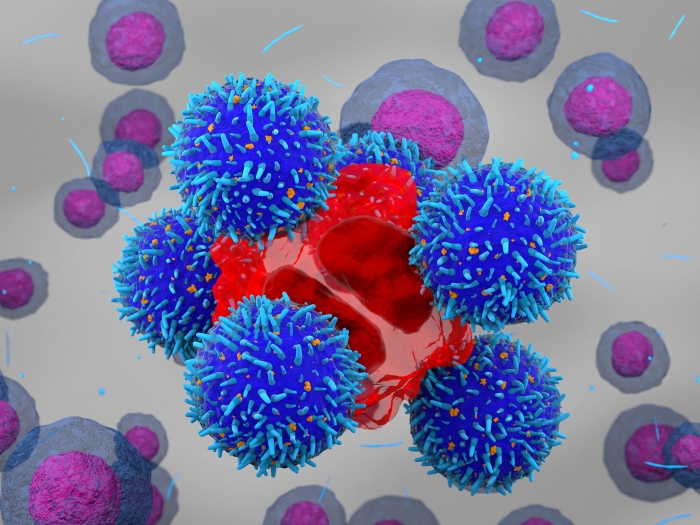
This type of tumor is compatible with immunotherapy, a treatment that uses the drug pembrolizumab (“Pembro”) to activate the patient’s own immune system to combat cancer. The mutating cancer cells produce a large number of proteins that the immune system detects as abnormal and targets for attack.
Krauss describes immunotherapy as “the future of cancer treatment” for those who qualify.
SEE ALSO: Immunotherapy: The Future of Cancer Treatment
“The miracle is that you can give a small amount of protein that unlocks the patient’s own T-cells (immune response cells) against the tumor,” said Krauss.
“The infusion of Pembro is like a private detective,” Kat said. “Pembro goes through your system, finds the cancer, and says to your immune system, ‘here it is, go get it!’
“It’s proving that your immune system is just as capable, if not more capable of attacking cancer cells than any chemical we can develop,” she added.
Minimal side effects
After receiving immunotherapy infusions every three weeks for 11 months, the only side effects Kat experienced were fatigue and brain fog.
Immunotherapy lacks the toxic side effects associated with chemotherapy, which causes nausea, vomiting and hair loss, Krauss said. Chemotherapy targets all rapidly dividing cells, which means the non-specific cell killing can also damage nerves and muscles.
Immunotherapy side effects can vary but overall are minimal compared to chemotherapy.
A small amount of people will have severe side effects where the activated immune system attacks your own organ systems, Krauss says. Some people will have more mild general immune system reactions like psoriasis while others may only experience fatigue and brain fog side effects.
Coping with the diagnosis
Kat’s mantra during treatment became, “I got this."
Her coping mechanisms included acupuncture twice a week, reflexology, gentle workouts, massages, daily meditation, a gratitude list and a “titanium rolodex” – a small group of people she could count on no matter what.
She turned off the news and turned on Seinfeld. “Keeping my sense of humor really helped,” said Kat.
Kat’s tumor nearly blocked her colon, which made eating a challenge. After a meeting with a dietician at Michigan Medicine, Kat ate soup for the first six months of treatment.
“My wonderful husband made all kinds of soup. We had to go out and buy a Vitamix so we could puree ingredients to the point of water.”
Remission and surgery
Throughout treatment, the MRI results kept coming back better and better.
After about 11 months of immunotherapy treatments, imaging indicated the tumors were in remission. Surgery was necessary to investigate if any tumors were active and to remove scarred tissue.
Two surgical oncologists, colon and rectal surgery specialist Gifty Kwakye, M.D., M.P.H., and liver and pancreas specialist Clifford Suhyun Cho, M.D., worked together on Kat’s case.
In surgery, Kwakye and Cho found scarring but no active tumor.
“The immunotherapy wiped out every single cancer cell,” said Krauss.
Who qualifies for immunotherapy?
“There’s been an explosion of using immunotherapy to treat certain cancers in recent years,” said Krauss.
Eligibility hinges on tumor type, shape and the proteins the tumor expresses.
Melanoma is more amenable to immunotherapy than most other cancers, says Krauss. For stomach cancer, esophageal cancer and lung cancer, immunotherapy is given in addition to chemotherapy.
For colon cancer, tumors with high microsatellite instability, like Kat’s, have a major response to immunotherapy – about 60% to 70% of people respond. Other tumor types are not as susceptible to the treatment.
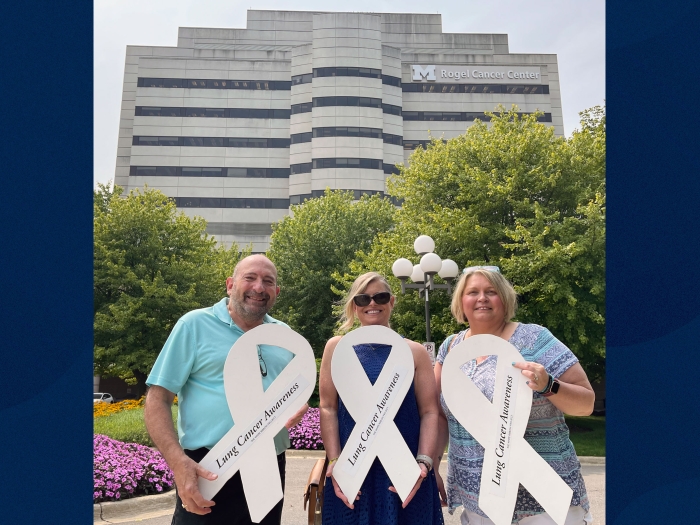
Rogel Cancer Center scientists continue to work with clinical researchers to develop new immunotherapy approaches to expand its success to a larger number of patients.
Giving thanks
Kat said she’s grateful for “living so close to Michigan Medicine” and the incredible caregivers she met throughout her treatment. She describes Krauss and physician assistant Pamela Christine Fisher, PA-C, as “outstanding, like no other team I’ve ever met.”
During her infusion treatments at the Brighton Center for Specialty Care and West Ann Arbor Health Center, she recalls laughing and talking with the “wonderful infusion nurses.” While at the hospital for surgery, she was thankful for the nursing staff who were “in command of the situation and completely took over my worries.”
Since treatment, Kat says she “lives her life in color,” from the colorful clothes she wears to her upbeat sense of humor.
As Kat recovers from her surgery, she’s returning to her work as a therapist/coach and slowly taking on more clients. She also spends her time writing her memoir, re-engaging with friends after her long recovery, traveling with her husband, Lars, and visiting her daughter Beth, in Chicago, and Kate, in Ann Arbor.
“I live a miracle every day,” said Kat.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!