Learn more about this important screening and the newer kid on the block: HPV testing
5:00 AM
Author |

With new guidelines come new conversations.
Elizabeth Campbell, M.D., an obstetrician gynecologist at University of Michigan Health Von Voigtlander Women’s Hospital, says she seems to have the same discussion over and over with new patients.
They are unsure if their previous OB-GYN ordered a human papillomavirus screening (HPV) test or conducted a Pap smear – or both, a co-test – to check for cervical cancer or abnormal cells that lead to it.
Both are done by collecting cells from the cervix but are tested differently in a lab.
While the most recent guideline change for cervical cancer screening was in 2021, Campbell has found that many individuals who were female at birth still believe they are only getting a Pap smear.
“Similarly, I think some people think every time they have a pelvic exam, they’re having a Pap smear done,” Campbell said.
OB-GYNs often use a speculum to observe the cervix without taking a cell sampling for the Pap smear or HPV screening. Patients may not know that and mistakenly think they are undergoing more formal screening.
Patients should ask what screenings they are getting and know the current recommendations, Campbell says.
Nearly 14,000 new cases of cervical cancer will be diagnosed in the United States in 2023, the American Cancer Society estimates.
What’s the difference between a Pap smear and an HPV test?
A Pap smear looks for abnormal cells in the cervix. It’s named after physician George Papanicolaou, an immigrant from Greece who discovered it in 1928, but wasn’t published until 1943.
Once one of the most common causes of cancer death among American women, the death rate from cervical cancer dropped significantly with the increased use of the Pap smear, the American Cancer Society reports.
HPV is a broad infection category and certain high-risk subsets of it have been linked to cervical cancer. An HPV test looks for those subsets. Even if you’ve had the HPV vaccine, you should continue to be screened for the virus, Campbell said.
How often should you have a Pap smear?
The guidelines from the American College of Obstetricians and Gynecologists recommend:
- If you’re younger than 21: No screening is needed
- If you’re 21–29: Have a Pap smear alone every three years. HPV testing can be considered for women who are 25–29, but Pap smears are preferred.
- If you’re 30–65: You can choose one of three options:
- Have a Pap smear and an HPV test (co-testing) every five years
- Have a Pap smear alone every three years
- Have an HPV test alone every five years
- If you’re 65 or older: No screening is needed if you have zero history of cervical changes and either three negative Pap smear results in a row, two negative HPV tests in a row, or two negative co-test results in a row within the past 10 years. The most recent test should have been performed within the past three or five years, depending on the type of test.
Should sexually active teens have a Pap smear?
Years ago, Pap smears were done on teens, but not anymore.
“It would be extremely unlikely for them to develop anything significant before they turn 21,” Campbell said.
“In addition, younger individuals, if they are exposed to HPV, are much more likely to clear that virus and not have it result in anything that's significant as a risk for cervical cancer.”
Your immune system will often clear HPV over time, she adds.
What are the exceptions to veer from the Pap smear guidelines?
Your medical history dictates if you continue screening annually, Campbell says. Those who should continue include those with:
- The human immunodeficiency virus, commonly known as HIV
- A weakened immune system
- A history of cervical cancer or cervical dysplasia
- Exposure to diethylstilbestrol before birth
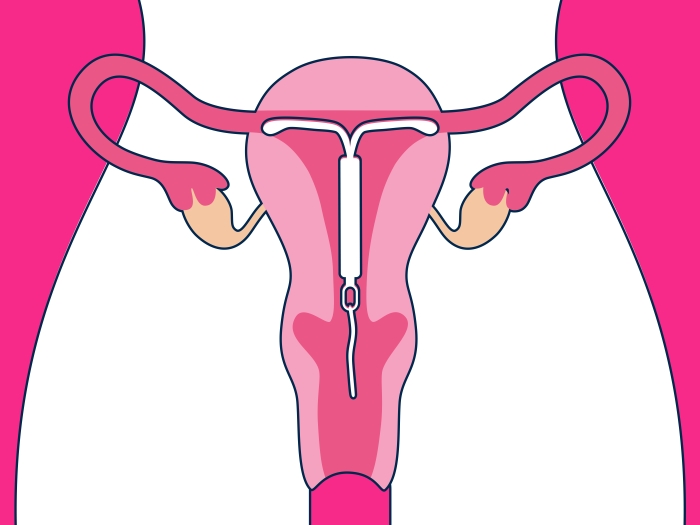
Is a Pap smear necessary after a hysterectomy?
It depends on the type of hysterectomy.
A total hysterectomy removes both the uterus and cervix. A supracervical hysterectomy, or partial one, removes the uterus but not the cervix. Knowing which one you’ve had will help with your long-term health care planning.
Patients who’ve had a total hysterectomy no longer face a risk of cervical cancer.
The only exception in those cases would be patients who had a hysterectomy done for either cervical pre-cancer or cancer. They should continue to have Pap smears of the vagina to check for vaginal cancer.
“Like which cervical cancer screenings they’ve had, another area that sometimes people are not quite clear on is the (type) of their surgery,” Campbell said.
How does menopause impact Pap smear testing?
Pap smears continue in menopause.
“After women go through menopause, they're at the highest risk for developing cervical cancer, which is age 40 to 50 and above, so it’s important for those individuals to still have that screening,” she said.
How should you prepare for a Pap smear?
Getting a Pap smear used to be riddled with rules. That’s no longer the case, Campbell says.
You may have a Pap smear when you’re on your period. You no longer need to abstain from intercourse two days prior to a test.
“They should not impact the ability or the interpretation” of a Pap smear, she said.
“Some women mentally prepare that they're going to have a pelvic exam,” Campbell said. “For some people, it takes a long time to be ready for that, which I totally get. But otherwise, there are no restrictions any longer.”

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!